Where Is My Pelvic Floor?
Your pelvic floor is a group of muscles and connective tissues that play a crucial role in supporting your bladder, bowel, and uterus. For many, the pelvic floor isn’t something you think about until you experience issues. However, understanding this important part of your body can help you take proactive steps to maintain its health.

Our pelvic floor plays an essential role in supporting our body’s daily functions. It acts as a foundation, holding up and stabilizing key organs like the bladder, bowel, and uterus. This support becomes even more significant when you consider the pressure constantly exerted on it.
In addition to bearing this load, the pelvic floor works in harmony with the surrounding core muscles, including your abdominal, diaphragm, and back muscles. Together, they create a coordinated system that provides strength, balance, and stability for your entire midsection. This collaboration is what allows you to perform everyday movements—like walking, sitting, or bending—comfortably and efficiently while protecting your pelvic organs from strain.
What muscles make up my pelvic floor?
The pelvic floor is a group of muscles and connective tissues that form a supportive hammock-like structure in the pelvis. The main pelvic floor muscles include:
- Pubococcygeus (PC) muscle: This is the largest and most well-known muscle of the pelvic floor. It stretches like a sling from the pubic bone to the coccyx (tailbone) and forms the bottom of the pelvic cavity.
- Iliococcygeus muscle: This muscle lies next to the pubococcygeus muscle and is also part of the levator ani muscle group. It extends from the ischial spine (part of the pelvis) to the coccyx.
- Coccygeus muscle: This muscle is also known as the ischiococcygeus muscle. It is located behind the iliococcygeus muscle and attaches from the ischial spine to the coccyx.
- Levator ani muscles: The levator ani is a group of muscles that consists of the pubococcygeus, iliococcygeus, and coccygeus muscles. These muscles provide support to the pelvic organs, including the bladder, rectum, and uterus (in females).
- Obturator internus muscle: Although not part of the levator ani muscle group, the obturator internus muscle contributes to the pelvic floor. It runs from the inside of the pelvis to the greater trochanter of the femur (thigh bone).
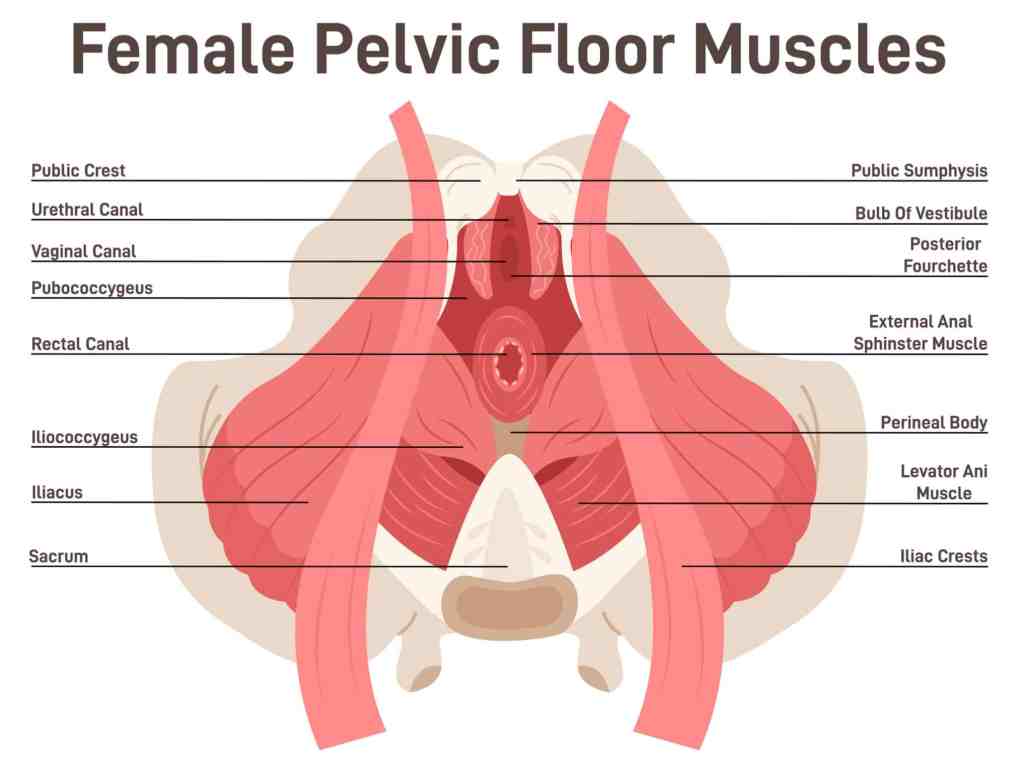
It’s important to note that the pelvic floor is a complex structure, and there are other muscles, ligaments, and connective tissues that work together to support the pelvic organs and maintain continence.
What is the purpose of my pelvic floor?
It’s easy to picture your pelvic floor as a hammock strung across two trees and imagine it acting as your pelvic floor supporting and holding you up. If the hammock stretches or tears, it isn’t able to support you comfortably or at all.
In reality, the pelvic floor acts more like the water in a dock that provides support to a boat, serving as a vital foundation for your pelvic organs. In this analogy, the anchors represent the ligaments and muscles that uphold and secure everything in its proper position.
If the water level is low, indicating a weak pelvic floor, the risk of organ prolapse increases as the organs may descend or shift from their optimal positions. Conversely, when the water level is high, or the muscles are excessively tight, or overative, the anchors experience tension and stretching, resulting in discomfort or pelvic floor pain.
This dynamic balance of strength and flexibility in the pelvic floor is essential for maintaining proper organ function and overall pelvic health.
What are some common pelvic floor issues?
Some common pelvic floor issues include:
- Stress urinary incontinence
- Urge urinary incontinence
- Mixed urinary incontinence
- Pelvic pain
- Chronic pelvic pain (CPP)
- Pelvic organ prolapse (POP)
- Bowel constipation
Pelvic floor muscle dysfunctions manifest when the muscles or connective tissues in the pelvic area are unable to perform their functions optimally. These dysfunctions can arise due to various reasons.
One common issue individuals may experience is the inability to relax their pelvic floor muscles properly. This could result from factors like chronic tension or a lack of awareness about how to release and unwind these muscles effectively.
On the other hand, some people may encounter problems arising from soft tissues that have been stretched beyond their optimal range and have become overly lax. Such overstretched tissues may struggle to provide adequate support, leading to a range of discomforts and dysfunctions in the pelvic region.
Both of these scenarios highlight the importance of maintaining a healthy balance of muscle tone and tissue elasticity within the pelvic floor. Addressing and managing these dysfunctions often involve specialized exercises, therapies, and guidance from healthcare professionals who specialize in pelvic floor health.
Pelvic Pain
Pelvic pain is characterized by discomfort occurring specifically in the pelvic region. It can stem from various systems within the body, including the urinary, digestive, and reproductive systems.
When pelvic pain is attributed to chronic pelvic floor dysfunction, individuals may experience burning and pain while urinating or during bowel movements. Sitting or standing for extended periods of time can also be painful, as well as activities such as inserting a tampon. Additionally, pain may be present before, after, or during sexual intercourse, impacting one’s overall quality of life.
Chronic pelvic pain often begins with physical symptoms caused by an injury, such as strained muscles, overstretched tissues, or organ-related issues. However, over time, the pain can evolve into a central pain syndrome, where the nervous system becomes hypersensitive, amplifying pain signals even when the original injury has healed. Managing this type of pain often requires a multidisciplinary approach, including physical therapy, pain management strategies, and sometimes counseling or mental health support to address the emotional and psychological aspects of living with chronic pain.
By restoring the proper functioning of the pelvic floor muscles and connective tissues, individuals can improve their overall well-being and alleviate the associated symptoms and challenges.
How do I prevent pelvic floor dysfunction?
Prevention is key! Do everything within your ability to keep your pelvic floor healthy. Being physically active and eating a healthy diet are some ways to help you prevent pelvic floor dysfunctions.
It is crucial to seek medical attention when experiencing pelvic pain of unknown origin. Consulting a healthcare professional can help determine the underlying causes and facilitate appropriate diagnosis and treatment. Identifying the source of pelvic pain is essential in order to alleviate discomfort, manage symptoms effectively, and promote overall well-being.
Seek medical attention and get formally assessed and screened for pelvic floor dysfunction. Some other professionals that you can work with and add to your pelvic floor dream team are:
- Medical Professionals
- MD
- OB/GYN
- Urologist
- Gastroenterologist
- Chiropractic
- Therapy
- Physical Therapist
- Occupational Therapist
- Sex Therapist
- Mental Health Counselor
- Complementary Care
- Personal trainers
- Health coaches
- Massage therapists
- Acupuncturist
- Dietician
This list does not encompass all the disciplines that can provide assistance in managing pelvic pain. It is important to recognize that there are various healthcare disciplines that can offer valuable support and expertise. The key aspect to consider is finding professionals who possess the necessary knowledge, experience, and personal understanding to address your specific needs effectively.
Finding experts who have a comprehensive understanding of pelvic pain and its underlying causes. You can receive individualized care that caters to your specific condition.
Disclosures & Disclaimers
Hey there! Just a heads-up. When you click on my links and make a purchase, I might get a tiny commission. It doesn’t affect my honest reviews and comparisons one bit! I’m all about recommending stuff I’ve personally tried, genuinely love, thoroughly researched, and wholeheartedly endorse.
** The views and opinions expressed on this site belong to Vigeo Ergo Consulting LLC. Any advice or suggestions offered herein are not a replacement for medical advice from a physician or other healthcare professional. My blogs are for informational and entertainment purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment.
Leave a comment